Regenerative Stem Cell Therapy
Why choose Regenerative Cell Therapy ?
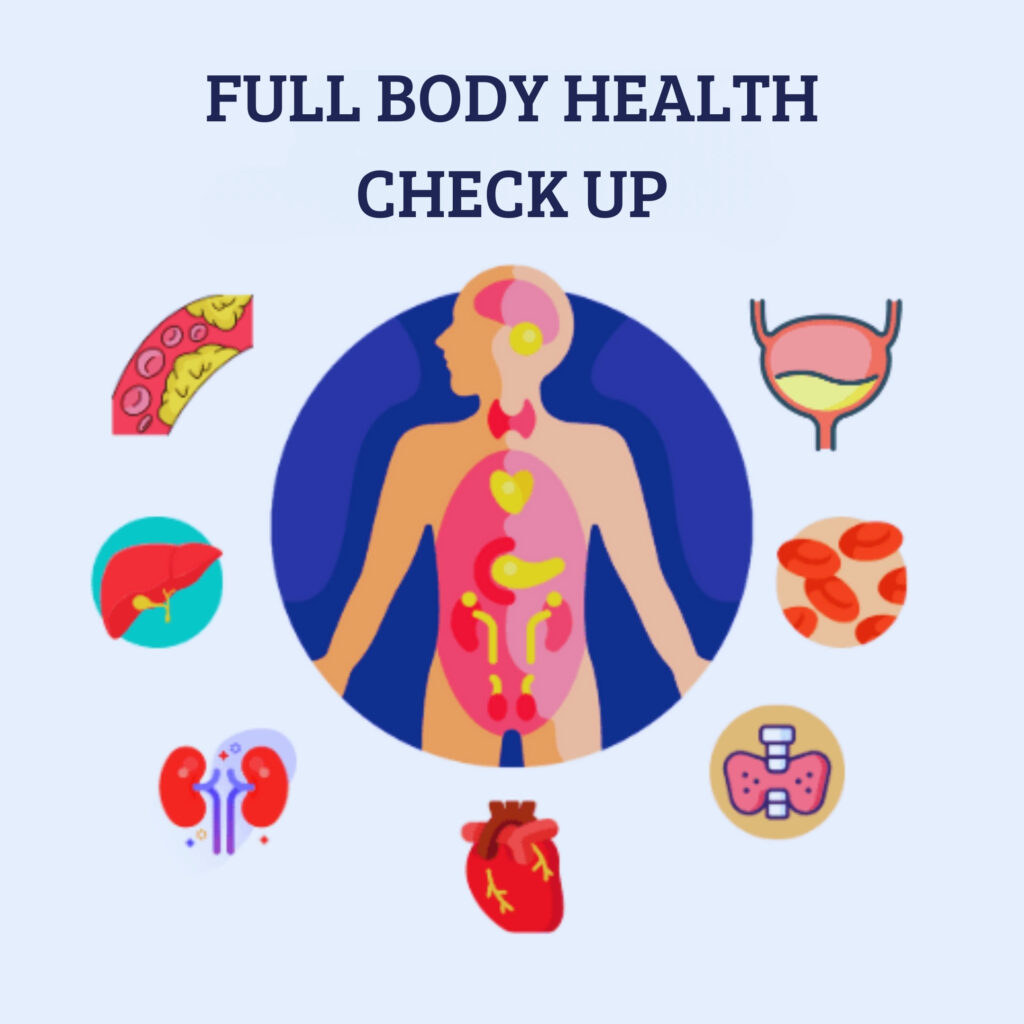
Stem cell treatment is a minimally invasive therapy that uses the power of your own body to help you heal from chronic inflammation and other illnesses. Our stem cell professionals at The American Institue of Regenerative and Cellular Research (AIRCR), will first do a thorough medical examination so they can have a greater knowledge of your current health status.
Once we gain a better understanding of your current condition and we can confirm that you’d be a good candidate for stem cell therapy – our physicians will prescribe a treatment protocol that best suits your needs for your current state. Each patient is treated as an individual – and no two protocols are the same. Additionally, our stem cell therapy doctors undergo frequent training and stay up to date with best practices in order to provide effective treatments to our patients.
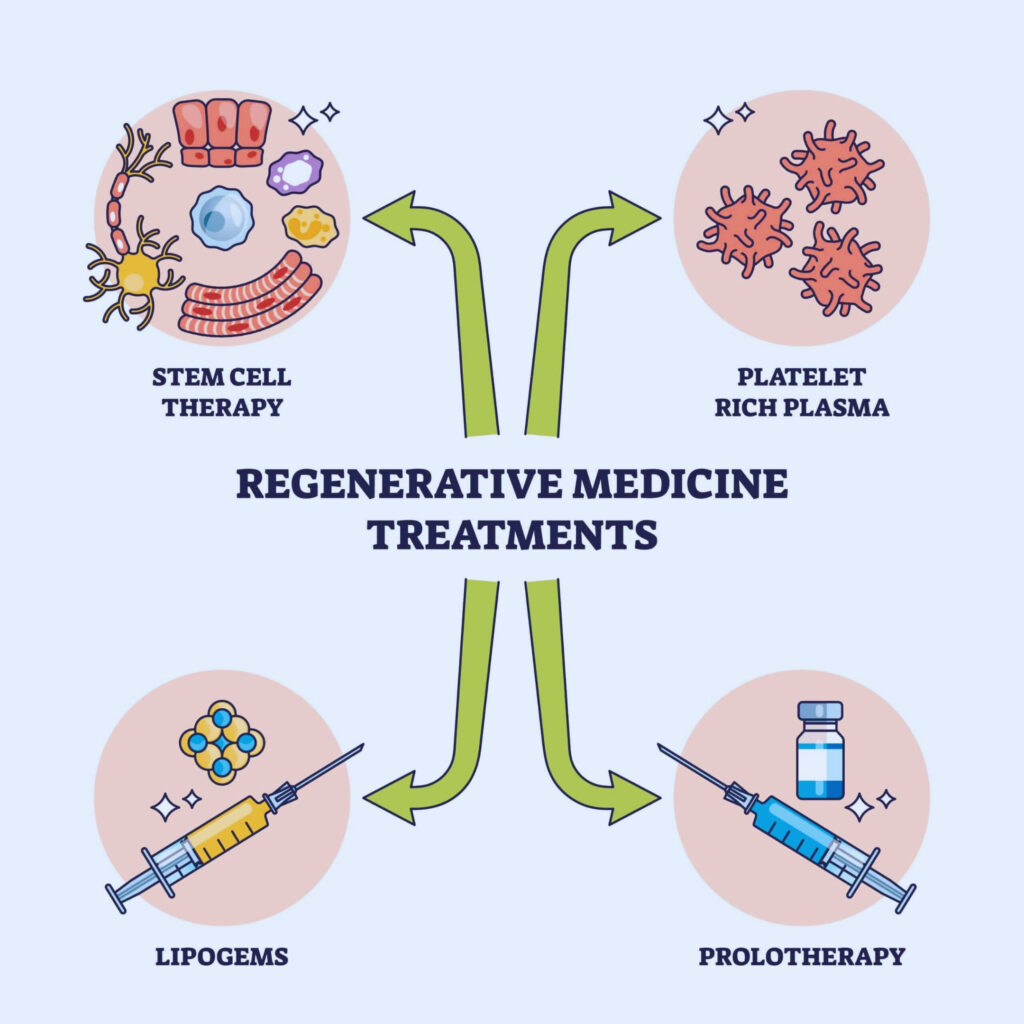
What is Regenerative Cell Therapy? and how does it Work?
Our body is made of trillions of cells, they are designed to perform a specific task within the body. For instance, red blood cells transport oxygen throughout the body, muscle cells help grow and repair muscle tissue and epithelial cells create the layer of skin.
When these cells degrade or die, it is the job of “unspecialized” regenerative cells to produce new cells. These regenerative cells are considered “unspecialized” cells because they don’t have a defined job. Instead, these regenerative cells have the ability to mature and differentiate into multiple types of cells, including cells that form bone, tendon, ligament, cartilage, muscle and meniscus. In addition, these regenerative cells can self-renew, producing even more regenerative cells. This They can even prevent other cells from dying due to lack of oxygen and they can produce anti-inflammatory proteins.
Stem Cell Therapy is currently being offered, and it is important to note that it’s still an ongoing research and is FDA approved
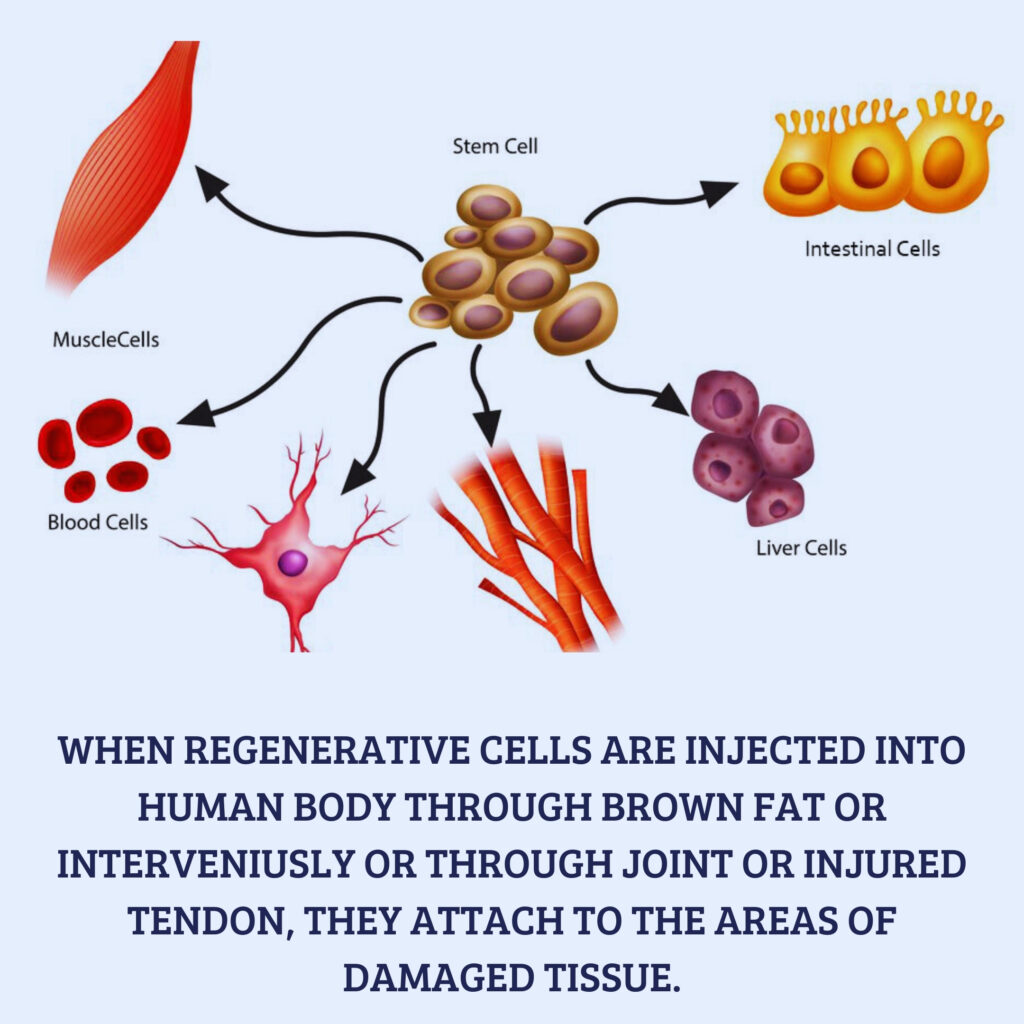
When regenerative cells are injected into human body through brown fat or intravenously or through joint or injured tendon, they attach to the areas of damaged tissue. The cells are able to sense the microenvironment of the damaged or inflamed tissue or injury area to determine what kind of cells to grow and what molecules are needed to enhance tissue healing. The stimulated regenerative cells begin to grow new cells and also act as your body’s own natural drug store producing and releasing the right combination of growth factors and proteins to stimulate healing and new growth of cell/tissue, cartilage, tendon and other organ systems.

Am I a candidate?
You may be wondering if you or a loved one is a good candidate for a stem cell transplant or cellular therapy procedure. Only your healthcare team can make the final determination. Our expert transplantation team works with you to determine your candidacy. The evaluation process includes many tests which may include:
- Thorough physical examination and review of your medical history
- Blood tests
- Imaging scans, including chest X-rays and computed tomography (CT) scans
- Tests to check your heart, lung, and other organ functions
- Bone marrow biopsy (removing a small piece of your bone marrow for analysis), which gives us a deeper understanding of your condition
- Psychosocial evaluation
- Stem cell transplantation is the standard of care for patients with certain types of cancer and blood disorders.
- Acute and chronic leukemias
- Aplastic anemia
- Multiple myeloma
- Non-Hodgkin and Hodgkin lymphoma
- Myelodysplastic syndromes
- Myeloproliferative disorders
- Primary light chain amyloidosis
- Sickle cell anemia
Who is a Good Candidate for Stem Cell Therapy?
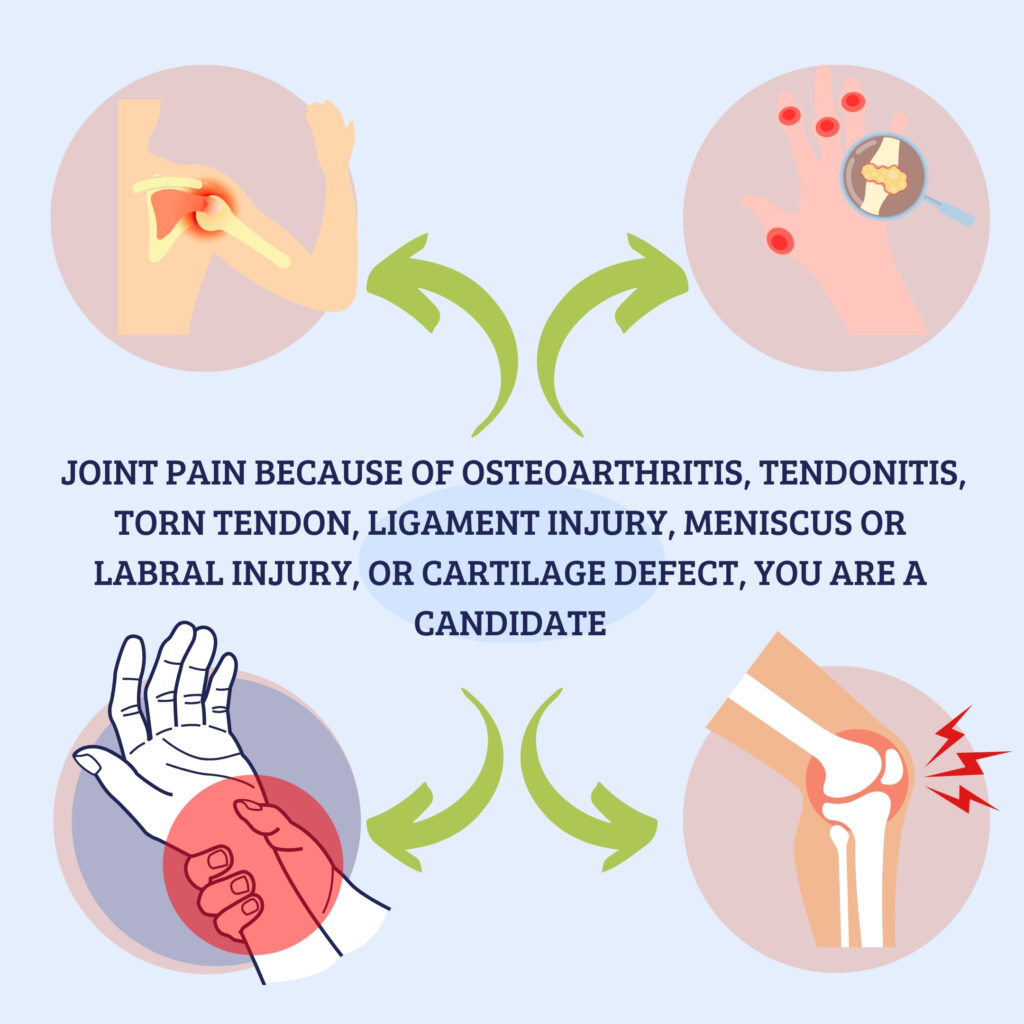
You may be a good candidate for stem cell therapy if you have been suffering from joint pain and want to improve your quality of life while avoiding complications related to invasive surgical procedures.
How do I know if I am a candidate for Regenerative Cellular Therapy?
If you are suffering from joint pain because of osteoarthritis, tendonitis, torn tendon, ligament injury, meniscus or labral injury, or cartilage defect, you are a candidate for regenerative cellular therapy using adipose tissue transfer. You are also a candidate if you want to restore joint cartilage and delay worsening of arthritis. There is no age limit for this procedure.
If you are suffering from joint pain because of osteoarthritis, tendonitis, torn tendon, ligament injury, meniscus or labral injury, or cartilage defect, you are a candidate for regenerative cellular therapy using adipose tissue transfer. You are also a candidate if you want to restore joint cartilage and delay worsening of arthritis. There is no age limit for this procedure.
Following an evaluation including discussing your history, performing a physical exam and reviewing x-rays and potential advanced imaging, a determination can be made whether or not regenerative cellular therapy is an appropriate treatment option for you. You may not be a good candidate for regenerative cellular therapy if you are currently being treated for cancer, have an active infection, take high dose Coumadin (warfarin) or have multiple medical issues. Dr. Steve Meyers does not perform regenerative cellular therapy into the spine for back or neck pain.
Why Consider Having Regenerative Cellular Therapy?
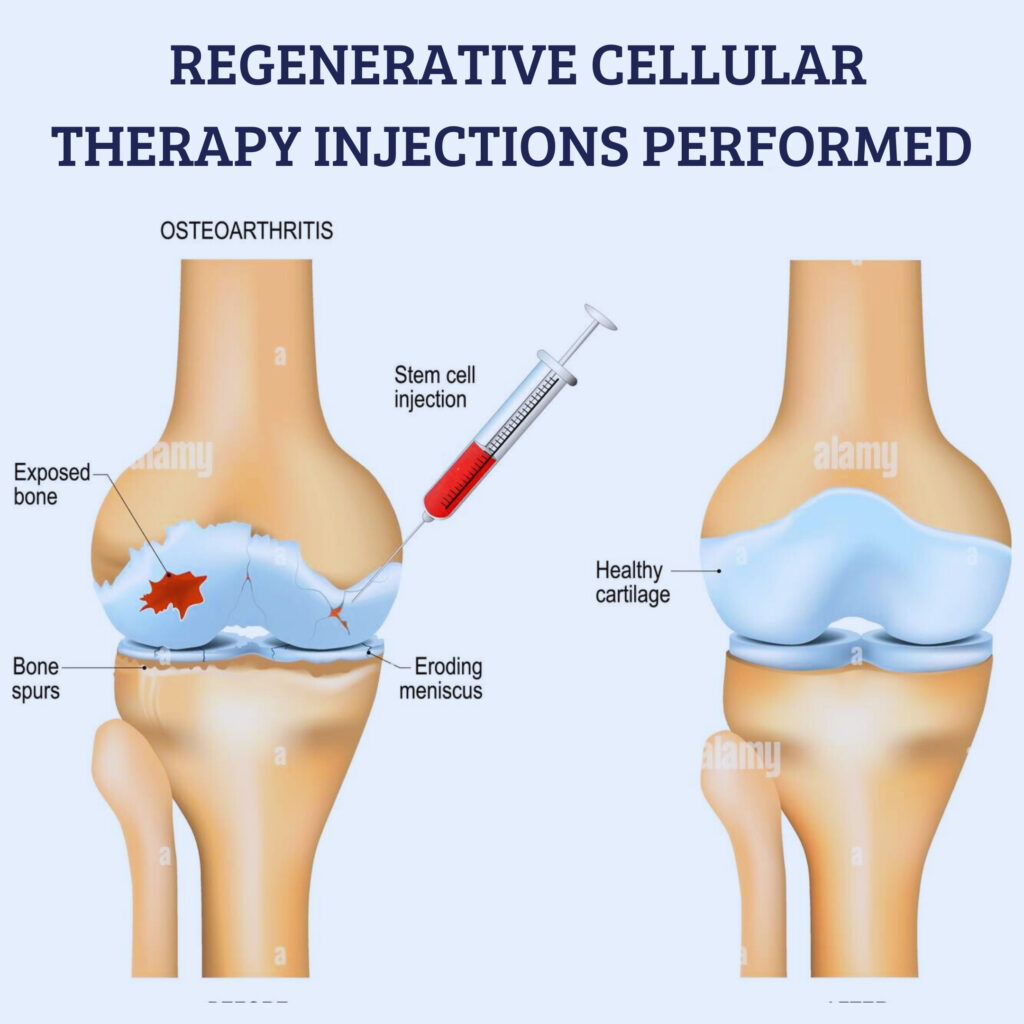
Osteoarthritis is a progressive degenerative problem without a cure. Over time, the thickness of cartilage that cushions joints continually decrease. In addition to significant potential side effects, typical treatment options for OA do nothing to restore cartilage or correct the problem. Repetitive steroid injections — despite providing temporary relief from pain — can actually worsen arthritis. The goal of regenerative cellular therapy for arthritis is to reduce pain and improve function by regenerating cartilage tissue and reversing some of the damage in the joint.
Many patients choose regenerative cellular therapy because they want to restore lost cartilage and delay worsening of their arthritis. Some choose regenerative cellular therapy because conventional treatments with NSAIDs, steroids or Visco supplements (Synvisc, Euflexxa, Supartz) have failed to provide adequate relief. For others who are looking to avoid surgery, prolong the need for surgery or who are not good candidates for surgery, regenerative cellular therapy provides a great treatment alternative.
Other patients choose regenerative cellular therapy to treat tendon/ligament injuries, plantar fasciitis or meniscus tears that have failed improvement with conventional treatment.


Why Use umbilical cord blood derived stem Cells instead of Fat or Bone Marrow?
fat tissue (adipose) and Bone marrow was the first body tissue used in medicine to obtain regenerative cells. Recently, however, umbilical cord blood (UCB) derived stem Cells has become the preferred source of regenerative cells for multiple reasons. UCB is one of the richest sources of regenerative cells with over 500 times more concentration of regenerative cells than bone marrow.
How do I know if I am a candidate for Regenerative Cellular Therapy?
If you are suffering from joint pain because of osteoarthritis, tendonitis, torn tendon, ligament injury, meniscus or labral injury, or cartilage defect, you are a candidate for regenerative cellular therapy using adipose tissue transfer. You are also a candidate if you want to restore joint cartilage and delay worsening of arthritis. There is no age limit for this procedure.
Following an evaluation including discussing your history, performing a physical exam and reviewing x-rays and potential advanced imaging, a determination can be made whether or not regenerative cellular therapy is an appropriate treatment option for you. You may not be a good candidate for regenerative cellular therapy if you are currently being treated for cancer, have an active infection, take high dose Coumadin (warfarin) or have multiple medical issues. Our research physician and investigator does not perform regenerative cellular therapy into the spine for back or neck pain.
Fat tissue with regenerative cells, which rise to the top while being resized and cleansed.

Fat derived regenerative cells, ready for injection.

How are Regenerative Cellular Therapy Injections Performed?
Regenerative cellular therapy is a simple, non-surgical, 3-step process performed in the office setting with local anesthesia (you are not put to sleep).
- Obtain the fat tissue (usually from the lower belly or love handles): After cleaning and numbing the skin, a thin instrument is inserted into the fat layer. The fat layer is then injected with saline and anesthetic (numbing medicine). Once numb, a thin tissue harvester is inserted, and the fat is collected by lipo-aspiration. This takes only a few minutes and is virtually painless. About 3-4 tablespoons are removed, not enough to make a significant cosmetic difference.
- Fat tissue processing: The fat is transferred to a sterile device that gradually reduces the size of the fat clusters. The tissue is exposed to mild mechanical forces that further break up the fat tissue while maintaining the native microenvironment. The tissue is rinsed with sterile saline to remove blood and oil residues. The cellular injection is prepared from this remaining tissue.
- Injection of regenerative cells into the joint or damaged tissue: All injections are performed using ultrasound guidance to ensure accurate delivery of the cellular therapy to the area of injury. Depending on location, topical or injected anesthetic may be used to decrease injection pain.
The whole procedure takes about two hours. You will go home the same day.

What can I expect after Regenerative Cellular Therapy?
The procedure is done under local anesthetic to minimize any discomfort. Most patients tolerate the procedure very well and with minimal pain. The area of fat harvesting may bruise significantly. For the first two to three days after the procedure, the joints or areas injected typically become swollen, stiff and painful. It can be difficult to get around these first few days. You do not have to sit around the house all day, but most patients will not feel like walking around the mall or exercising. You will be given a prescription for pain medicine to help with these early symptoms. Typically, four to seven days after the procedure you can resume normal activities. You will be instructed to begin a home exercise program to enhance treatment results. NSAID medications such as ibuprofen, Advil, Motrin, Aleve, Celebrex and Mobic need to be avoided ideally for eight to 10 weeks after the procedure as they can block the regenerative process.
Improvement after regenerative cellular therapy does not happen overnight. Growing new cells and healing tissue takes time. Most patients see mild improvement at one month. But significant improvement can take two to three months and sometimes longer.
Is Regenerative Cellular Therapy Safe?
Research and clinical data show that regenerative cellular therapy is extremely safe with minimal risk for any adverse reaction or complication. Because the injected cells are produced from your own body, there is no concern for rejection or disease transmission. There is a small risk of infection from any injection or lipo-aspiration, but this is very rare.

What is the Success Rate of Regenerative Cellular Therapy?
Multiple clinical research papers conclude that regenerative cellular treatment significantly improves pain and function in addition to increasing cartilage volume and quality on MRI imaging. According to published research, regenerative cellular treatment for knee arthritis results in 58-68% improvement in pain and 67-83% improvement in function one to two years after treatment. Most of this improvement occurs in the first three to six months. Tendon and other soft tissue injuries can respond even better. Studies describing longer-term success with regenerative cellular therapy are currently unavailable. Hopefully the treatment will provide multiple years of improvement, if not a permanent cure.
Does my insurance pay for Regenerative Cellular Therapy?
Unfortunately, even though it is highly effective, regenerative cellular therapy is considered by insurance companies to be experimental and investigational. Therefore, no insurance covers the cost of this treatment. CareCredit is accepted if a payment plan is desired. For more information on payment plans to finance the procedure please visit: www.carecredit.com


What is the cost of Regenerative Cellular Therapy?
The cost of regenerative cellular therapy is $4,000 for a single joint or injury. Additional joints/injuries can be treated at the same time for as little as $800. Paying more for treatment does not mean that it will work better! Outcome is dependent on multiple factors including having the correct diagnosis, proper harvesting technique, processing that maximizes growth factor and reparative potential and, of course, accurate delivery to the site of injury.
